The fall happens fast. One moment, I’m walking down the stairs at the gym; the next, I’m moving through space.
I land to the sound of bone snapping.
Within minutes, a flurry of personal trainers is around me, helping me limp over to a weight bench and prop up my leg. The irony is rich that I’ve injured myself walking down the stairs, not doing some bionic box jump or high-speed treadmill run, which I don’t do anyway.
“I think you broke it,” one says, biceps bulging beneath his t-shirt.
“Definitely,” the other says, his face aglow with health.
Soon, my ankle is Gothically swollen. I call an Uber. They help me to the door and navigate the slush outside and ease me into the car.
At Immediate Care, my ankle is x-rayed. The attending physician tells me my distal fibula is fractured. She puts the X-ray against the lightbox. It’s unmistakable: a piece of bone broken off in the blackness as if floating in space.
There’s no question the bone is broken. The diagnosis isn’t in doubt. We can see precisely that it’s the fibula, not the tibia.
In this, it’s so unlike the six mental health diagnoses I received over the past twenty-five years. No X-rays for those. No blood tests. Just doctors’ best guesses at how to define my bouts of depression, anxiety, confusion, exhaustion, obsessions, hyperactivity, compulsions, insomnia, panic, and suicidality (not all at once).
“The fibula isn’t a weight-bearing bone,” she says. “It supports and stabilizes. It keeps us steady. To heal, you need to immobilize your ankle.”
No doctor or mental health professional who leveled a psychiatric diagnosis ever mentioned healing.
Then it strikes me (slowly, dully) that I won’t be able to walk. “For how long?” I hear the panic in my voice. I’m already trying to heal from serious mental illness, and I’ve stopped taking Klonopin—just quit cold turkey, which is a terrible, terrible idea, as Dr. R will later inform me. The only relief from the constant hum in my chest is walking miles and miles—no matter how cold or snowy it is—as far as it takes.
“The orthopedic surgeon will give you a precise estimate for how long you’ll need to wear the boot,” she says, clearly not understanding the tragedy that’s just occurred.
“A week or so?” Even to me, what I’ve just asked sounds absurd.
“Um,” she draws out the word, “I’m going to guess it’s going to take longer than that.”
A nurse comes in with a huge, heavy, black orthopedic boot.
The physician’s tone is firm. “Don’t go walking around in it. When I say immobile, I mean immobile.”
“But I’ll be able to walk?” I ask as if she didn’t just say Don’t go walking around in it.
“The boot is support. A broken bone needs to remain stable. Otherwise, it won’t join or regrow properly. People try to push it, but that will just delay healing.”
I ask if I can walk a bit, just here and there, just—
“You can—if you don’t ever want to heal or walk again.” She opens the door to leave. “And keep it elevated even when you sleep. Maybe even sleep in the boot.”
*
People like to compare mental illnesses to physical illnesses. Type 2 diabetes is a favorite comparison. But the metaphor implies that psychiatric diagnoses like major depressive disorder and anxiety disorders and eating disorders and obsessive-compulsive disorder and attention deficit hyperactivity disorder are necessarily lifelong, which we know they aren’t.
One of the most valuable illness metaphors comes from Dr. Thomas Insel, a neuroscientist, psychiatrist, and the former director of the National Institute of Mental Health (NIMH).
When I interviewed him years after I broke my foot, he likened mental illness to breaking a bone. As with a broken bone, we can heal from every type of psychiatric diagnosis, even schizophrenia, which is often treated like a death sentence. Healing is a long, complex process, he explained. When the bone first breaks, it bleeds. Then it becomes inflamed. Only then does it begin to repair. Finally, it starts to heal, which can take months or years, sometimes as long as a decade. What’s most remarkable is that after a bone heals, the point of the break becomes the strongest part. It’s as if we become stronger for having broken it.
Some people with mental illness take issue with the broken-bone comparison because they think it’s simplistic and dismissive. But breaking a bone is a big deal, and Tom Insel isn’t saying that everyone will heal from mental illness, only some.
It’s not a perfect metaphor in other respects. We don’t, of course, have the equivalent of an X-ray to show that someone actually has the psychiatric diagnosis they’re given. Approximate diagnoses and treatments are all we’ve got. It’s a lot to ask of psychiatrists: Heal me even though you don’t what exactly is wrong or have the remedy or cure. Plus, the bone is only the strongest part for a short time. After recovery, we don’t reach some sort of blissed-out state of high-functioning happiness.
As with mental health recovery, recovery from a broken bone will actually look different for each person. Some will heal relatively perfectly. They’ll run marathons and ultra-marathons, forgetting they ever broke a bone unless reminded. For others, the bone won’t quite set right, resulting in chronic pain or a limp for which they need continuous care.
Ultimately, no metaphor suffices. Mental illness is unlike any other experience or condition. It’s brutal and excruciating and can be fatal. But as with a broken bone, it can also result in full recovery.
The diabetes comparison might actually be the best after all. There’s early evidence that type 1 diabetes, once said to be lifelong (no exceptions), is, in fact, curable. In a recent study, one participant’s daily insulin use decreased by 91 percent, and—this is the miraculous part—his body started producing insulin on its own. It’s early yet and the study used a very small sample, but it seems that a once-incurable disease is curable after all.
*
Sleeping in the boot borders on Medieval. It’s like a very mild version of being on the rack. The boot weighs down my leg, stretching the ligaments no matter what position I sleep in.
For the next few nights, insomnia becomes my closest companion. Each morning, in front of my computer, drinking coffee, the ice I put on my ankle numbs the pain but brings with it an icy burn.
I’ve been feeling the blackness, the unsteadiness, the sodden pit in my stomach, the hum in my chest again. They’d lessened, which I’d seen as proof that I was, in fact, healing from mental illness.
The hum in my chest intensifies. The refrigerator drones. My thoughts race on repeat: I’ll never heal. My foot will never heal. My mind will never heal. My brain will never heal. My brain is broken.
Within a week, hobbling in the boot has become familiar but no less tedious. I’m able to click along at a fairly good pace. This, of course, goes against the very point of the boot. The boot is meant to immobilize so my broken foot can heal.
I enter the waiting room of the osteopath I was assigned in Immediate Care. After checking in, I sit amidst the other patients. Some are in casts, others in braces, and others in splints. Some show no sign of having been injured.
According to Dr. Patel’s profile on the hospital website, he’s certified by the American Osteopathic Board of Orthopedic Surgery. Foot and ankle fractures are his specialties. He has eight hundred and twenty-three ratings which average 4.8 stars.
I never thought to find reviews of any of the psychiatrists I saw. One psychiatrist is connected to this same hospital. I look him up. His profile shows he’s certified by the American Board of Psychiatry and Neurology. His profile has no star ratings.
Another of my psychiatrist’s profiles is tied only to the private practice he’s associated with. It links to his CV, which is replete with licensures, certifications, trainings, honors, and awards. No star ratings there either.
My current psychiatrist, Dr. R, is also affiliated with this hospital. His profile doesn’t even have his photo. No bio, just where he got his Ph.D. and M.D. His profile lists his publications, the titles of which are so scientifically specific they’re like gobbledygook: DNA/RNA-binding protein, chick aggrecan, ubiquitin-mediated degradation. If I’d gone by his profile, would I have chosen him? Probably not, but he’s the best I’ve seen.
The nurse calls my name. I limp assertively behind her. She walks slowly to accommodate me. I want to tell her I’m fine. I’m healing. We can go faster.
She shows me to the examination room. Eventually, Dr. Patel comes in with a resident in tow. The resident looks so young he could be fresh out of college. Dr. Patel is handsome, confident but not arrogant, caring but brusque. The clock on our appointment time is clearly ticking. He clicks the keyboard, and soon the X-ray of my broken ankle is on screen. The two of them consult.
Dr. Patel helps me out of the boot, touches various spots, and asks me if it hurts. It does, but I don’t want to say so. I want out of the boot. I want to be healed.
“You don’t need surgery,” Dr. Patel says. “Six more weeks and we’ll see how you’re doing.”
Panic rises in my chest. “Six weeks in the boot?”
Dr. Patel explains his reasoning at length. I’ve torn ligaments too, and those take longer to heal. I look to the resident as if for help, but he just smiles.
Dr. Patel says I can get a second opinion. He says this easily and without malice.
A second opinion? In a couple of months, I’ll read advice from Dr. Allen Frances, one of the most powerful figures in psychiatry. In his book Saving Normal, he’ll stress the importance of getting a second opinion whenever you see a psychiatrist. I’d never thought of it. No one recommended that I do. This is, of course, a luxury, especially in our overcrowded mental health system, but I wish I had thought that way.
I shake my head. I trust Dr. Patel. It’s a feeling.
“You’ll be out of that boot soon enough,” he says.
As I hobble to the elevator, my foot seems to hurt more than it did when I came in. Six weeks. But it will heal. Dr. Patel said as much. You’ll be out of that boot soon enough. He’ll track my progress as my ankle goes from broken to healed.
*
What if one of my psychiatrists or therapists had spoken to me that way? You could be out of this depressive episode soon enough. You’re experiencing an intense bout of anxiety, but it is possible to heal. People have healed from bipolar disorder—not that it’s easy. ADHD can be resolved. Anorexia isn’t necessarily lifelong. No promises. Lots of could’s and can be’s and necessarily’s. Conditionals, but also possibilities.
During the twenty-five years I was in the mental health system, not one clinician gave me the recovery statistics of the diagnoses I received or explained the stages of recovery.
One recovery model, taken from the Transtheoretical Model of the Stages of Change, traces recovery as a nonlinear process in which a person moves from seeing themselves as a diagnosis whose life is limited to someone believing, committing to, and taking action to create the life they want. (Some people dislike this model because it’s so focused on taking action, which is both Puritan and capitalist, but there are other models.)
This model has five stages:
Stage 1—Impact of illness: the person is defined by stigma and the symptoms they experience and sees themselves as the diagnosis, which may or may not be helpful
Stage 2—Life is limited: the person glimpses but doesn’t think change is possible because they can’t imagine an identity outside of their diagnosis
Stage 3—Change is possible: the person has hope, yet still isn’t willing to take the risk
Stage 4—Committed to change: the person starts to take steps toward recovery
Stage 5—Action taken: the person no longer sees life as limited and trusts in themselves
These stages aren’t prescriptive; each person determines what each stage will entail and what the end goal will be.
But recovery wasn’t mentioned on WebMD. Or on the National Alliance for Mental Illness (NAMI) website. (NAMI wouldn’t have a webpage dedicated to it until 2021—though it’s excellent.) No media outlet—not The New York Times or the Washington Post—covered it. BP Hope, the bipolar magazine I depended on, said that bipolar disorder was physiological like heart disease and “can be managed but never goes away.”
Soon, I’ll learn that most of the time I spent in the mental health system, the U.S. government had embraced the recovery model over the biomedical model, which emphasizes that mental illness is biological and can only be managed.
Beginning in 1999, the government had called upon the psychiatric community to make the recovery model the core of our mental health system.
Recovery as a concept had gained traction with the passage of the 1990 Americans with Disabilities Act, which recognized serious mental illnesses as disabilities. Surgeon General David Satcher’s 1999 report on mental health was the first official policy to include the term recovery: “All services…should be consumer-oriented and focused on promoting recovery.… [T]he goal of services must not be limited to symptom reduction but should strive for restoration of a meaningful and productive life.”
News that a full recovery from mental illness was possible seemed to take hold with politicians at the turn of the twenty-first century. The President’s New Freedom Commission on Mental Health in 2003 called for a “profound change” on the federal level that would shift the focus of treatment toward recovery and protect the rights of adults with serious mental illness.
Its Executive Summary led with these words: “We envision a future when everyone with a mental illness will recover, a future when mental illnesses can be prevented or cured…” It promised a transformation “not at the margins of a system, but at its very core.”
*
The restaurant is crowded. Every table and every seat at the counter is full. My father and I stare down at the laminated menus. We’re at a four-top, so I can prop my foot on the extra chair. Condensation beads down our water glasses, forming rings on the table.
My broken foot and being in the boot are hampering my determination to recover from mental illness. I’ve lost the ability to go for the long walks that used to help calm and soothe me and make me feel like I was making strides toward recovering my mental health.
Even now, a hum pulses in my chest. The pit in my stomach is so heavy and black that it’s my whole being. The clank of plates being put in bus bins sounds as if it’s inside my head. The table next to us is too close. The two couples drink mimosas. Their voices are too loud though I can’t make out what they’re saying.
The server arrives, and we order. Out the window, the sunlight faintly lights the street. She brings my coffee, which I pour milk into and sip. The pulsing in my chest intensifies. I keep sipping.
Eventually, our food arrives. The skillet the server places in front of my father still sizzles. The omelet she puts in front of me is the size of my forearm. My father puts hot sauce on his eggs. I pick at my omelet.
He says, “I’m really sorry this happened to you, hon.” He means my ankle.
No one knows I’m trying to recover from mental illness. It’s being done in secret to prevent anyone from discouraging me. I tell him I’m going to get better, referring to my mental illness.
“Of course you are,” he says. “Just wear that boot.”
To be continued next week…
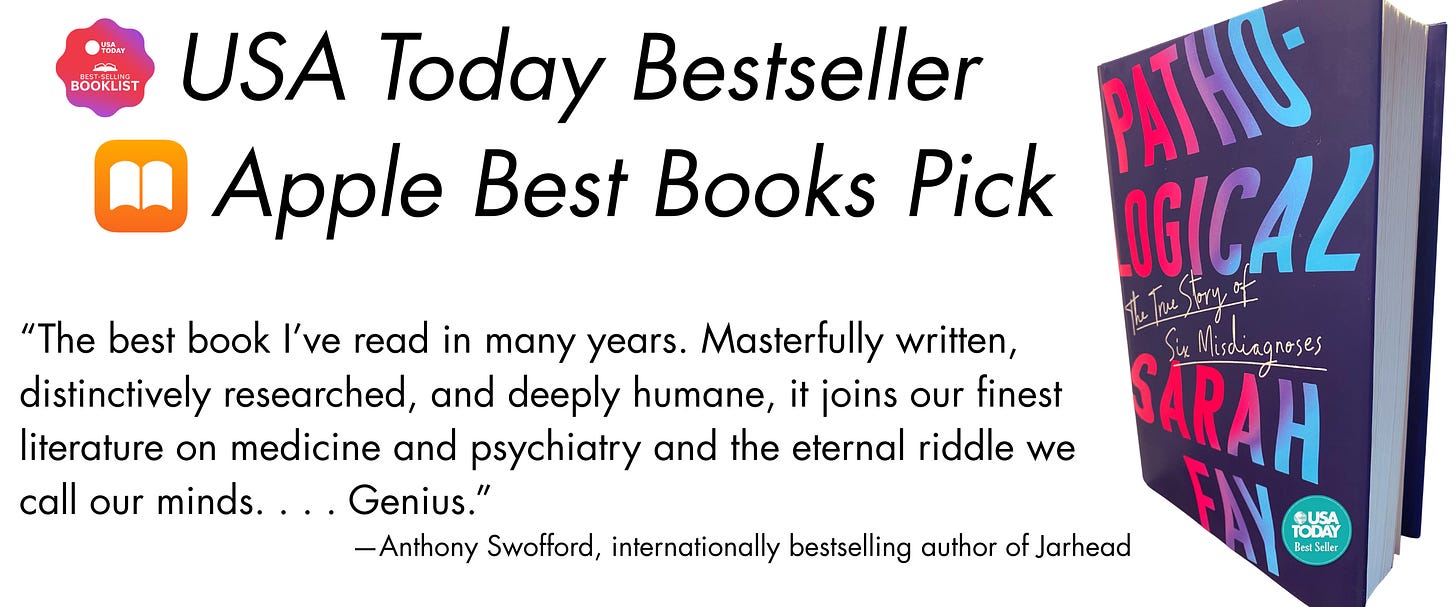
Thank you for reading! You can buy my journalistic memoir Pathological: The True Story of Six Misdiagnoses (HarperCollins), a USA Today bestseller that traces how we’ve come to believe that ordinary emotions are mental disorders. If you’ve already read it, thank you! You can gift a copy to a friend, your local library, or your favorite used bookstore.



Wow, what a post. Years ago during my pre-high-school period, I was forced to wear a cast on my left leg for a month (This was the result of me walking like a penguin and being not careful of slippery surfaces. Fortunately, it was during my end-of-year exams, and I had a lot of time for recovery). However, because of this, I had to skip a session of my English class at that time (I remember I told my mom: "Even if I crawl, I MUST go to that English class. Otherwise, I'd feel like I'm dying).
This June, before Israel's attack on Iran, my dad fell from a tree in our villa-garden and badly injured his left foot (in the hospital, the doctors wanted to make sure his tendons weren't injured. Luckily, his tendons were unharmed). To this day, sometimes he has trouble walking stairs, and his foot swells if he sits for a long time (My dad's not the type to sit for a long time).
Your story took me vividly through your feelings and thoughts during this journey. Thank you for sharing this on going experience. Really appreciate your comments about Neff and Brown, had those thoughts myself, thank you.