What Does Eighteenth-Century Paris Have to Do With the Cure for Mental Illness?
Answer: A lot.
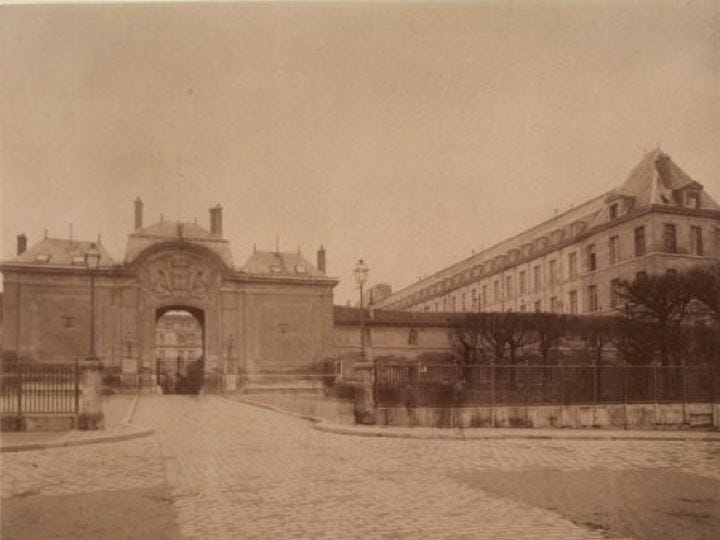
I like to imagine the Hospital Bicître in Paris in 1793.
The above sepia-toned photograph comes to mind: the cobblestone path leading to the arched entrance, the stone buildings stretching past the gates.
A century earlier, it looked more like a rural prison, which it was—in part.
It was part prison, part housing shelter, part mental asylum. Most patients were afflicted by dementia, syphilis, or paralysis.
In most asylums, “lunatics” were typically divided into aggressive and non-aggressive. They were physically abused and not given clothing. The first line of treatment involved chaining them to walls.
But that’s not what I think when I picture the Hospital Bicître because patients there were freed thanks to two men: Philippe Pinel, a physician, and Jean-Baptiste Pussin, governor of the hospital.
Pinel is credited with having liberated mental patients, for which he’s now often referred to as “the father of modern psychiatry,” but he learned from Pussin. As governor, Pussin found that patients fared better when (surprise!) they weren’t chained to walls.


Maybe I shouldn’t think so highly of Pinel and Pussin. Patients were still put in straight jackets and isolated.
But the two men revolutionized how people with mental illnesses were viewed.
Since the Middle Ages, the insane had been seen as degenerate, demonic, bestial, and alien. Pinel and Pussin changed that. They thought of them simply as people suffering from mental and emotional distress.
People with mental illnesses were seen ordinary human beings, albeit more sensitive to the world than others (qualities we sometimes value in artists and other “creatives,” as they’re now called), with rights like anyone else. Pinel and Pussin pushed for holistic care and developed traîtement moral (not to be confused with moral treatment, which came later in the U.S. and England). Traîtement moral had nothing to do with morality (right and wrong, good and bad); it asserted that those with mental illnesses (surprise!) shouldn’t be abused and should receive psychological care.
It worked. The hospital boasted a cure rate of 90 percent if—and this was a big if—patients were not treated at another hospital first.
Why?
Because Pinel and Pussin knew that physical abuse and the emotional toll of being denied your human rights and told you’re beyond help compounds mental illness and leads to further deterioration.
We worsen not because we have a mental illness but in response to how we’re treated.
Psychiatrists today don’t like the word cure, but curing mental illness isn’t the same as boasting of a cure. Cure comes from the Latin curare, meaning “to take care of someone.”
It wasn’t until the Middle Ages that cure was even associated with medicine and used as a noun to mean a remedy.
There’s no single cure for mental illness—no pill or magic bullet. The definition of the verb to cure is “to restore to health, soundness, or normality.” Those categories (health, soundness, or whatever we think of as “normality”) are abstractions determined by each person and culture.
Traîtement moral was rooted in the belief that patients could not only be cured but cured so entirely that they could return to the hospital and be employed to help others heal—an early example of what’s now called peer support.
Pinel even hired ex-patients to work at the hospital. Pussin—get this—had once been a patient at the hospital before he became governor (albeit for tuberculosis, not mental illness).1
In the scientific literature, Pinel introduced three pivotal truths that we still have trouble accepting some two hundred years later. Professor of Psychiatry at Yale Larry Davidson and his colleagues outline them in their excellent history of people healing from mental illness over the past two centuries, The Roots of the Recovery Movement in Psychiatry:
anyone can develop a mental illness;
mental illness occurs in response to external events (it’s not solely biological); and
it’s not all-encompassing, i.e., even in an acute phase, it merely influences a person’s perceptions, judgments, ideas, and reasoning (it’s not the whole person).
Think about it.
We still believe that only certain people suffer (read: the weak, the biologically flawed, etc.).
The chemical imbalance myth (yes, it’s a myth) and the biomedical model of mental illness continue to reign supreme.
Some people adopt diagnoses as identities as if having depression or anxiety or ADHD or schizophrenia infuses every part of them and their lives instead of being just one aspect of it.
Traîtement moral showed that mental illnesses can be episodic and aren’t necessarily chronic, something many clinicians still don’t either know or simply don’t encourage. Healing depends on restoring hopefulness to patients, yet from the most stigmatizing to the least, diagnoses are believed to be forever. “Symptoms” like depression and irritability and distractibility and anxiety and obsessions and compulsions, which are part of the human condition, supposedly represent a catastrophic brokenness in the brain. The American Psychiatric Association (APA) frames major depressive disorder, anxiety disorders, ADHD, OCD, bipolar disorder, and other diagnoses as “common” and likens them to heart disease or diabetes, implying they’re inevitably chronic, which they aren’t.
How can we heal if clinicians don’t encourage us to do so?
It turns out that very little encouragement is needed to create conditions for healing—not just in mental health but in all areas of health.
A 2018 study conducted by Stanford psychology Professor Alia Crum and her colleagues showed that a few comforting words from a physician speed healing. In the study, participants who were told that their allergic reaction would start to diminish and their symptoms would go away experienced relief and less itchiness than those participants to whom the doctor didn’t speak. Reassurance from a clinician induces the placebo effect, in which a person’s mindset influences recovery outcomes. A lack of support can produce a “nocebo” effect, in which a negative outlook leads to deterioration.
All we need is a word: possible. It’s possible to heal and create the life that’s best for us. Just maybe that’s the truth.
What would our mental health system be like if everyone knew that recovery from all psychiatric disorders is possible? What if we were taught the history of mental health recovery? What if they understood that in the 1980s, just when it seemed that the contemporary Recovery Movement would transform psychiatric practice forever, gearing treatment toward wellness, not a lifetime of illness, it both blossomed and met with near-movement-dissolving obstacles?
By that point, the Recovery Movement had its own national conference. It had gained more respect, leading to invitations to be involved in political events, psychiatric conferences, and lobbying efforts. It received more media attention, including two of the movement's leaders’ appearances on The Oprah Winfrey Show.
But it was also determined to remain outside the establishment. The movement wasn’t, as one of its leaders Chamberlin explained, anti-psychiatry. “Anti-psychiatry” is a theoretical debate waged by intellectuals. The movement believed in self-help, the premise that patients could determine their treatment and lives.
As the Recovery Movement gained momentum, different factions arose, each with its own goals and approaches. Ironically, the splintering within the Recovery Movement occurred because more people wanted to join in the fight for better treatment for people with mental illnesses.
Family members seeking secure services for their loved ones started their own movement. They eventually founded what would become the National Alliance for Mental Illness (NAMI), one of the most powerful mental health advocacy groups in the country.
Families didn’t fall in line with the goals and outlook of the Psychiatric Survivors Movement. While families questioned aspects of the mental health system but pleaded for more—or in some cases, any—resources, psychiatric survivors doubted that hospitals were beneficial at all, even in a crisis.
Like Pinel and Pussin, they knew that the longer patients remained in inpatient care, the more likely it was they would become “chronic” cases.
Psychiatric survivors did want to work with the government and other bureaucratic entities and believed psychiatry could be reformed. Patients, who they referred to as consumers to destabilize the power dynamic, needed transition programs that would assist them in moving from inpatient care to living and working in the community again.
Terminology was also a sticking point. Families adopted the term consumer when referring to patients. Survivors and ex-inmates like Chamberlin rejected the label. Although families said that consumer suggests having influence over the mental health system and inverts the typical power imbalance, Chamberlin reminded them that she’s a consumer when shopping for a refrigerator, not when being involuntarily committed.
Members of the Psychiatric Survivors Movement, particularly those who’d experienced horrific abuse while hospitalized and had since fully recovered, didn’t believe those without experience of mental illness could or should set goals and assume leadership roles. According to a 1990 article by Chamberlin, published in the Journal of Mind and Behavior, groups that let in mental health professionals and non-patients pivoted away from the movement’s militant liberation stance and adopted a reform-from-within approach, which went against their goals.
Politically and economically, the 1980s promised to deepen the mental health crisis. The strides made under the Carter administration during the 1970s didn’t last. The administration’s Mental Health Systems Act hadn’t answered all the issues like lack of access to services, neglect of those from marginalized groups, the shortage of clinicians, and the burden on families, but it attempted to establish the community mental health centers the country so desperately needed.
President Reagan had only been in office only seven months before repealing most of it. Although the Patients’ Bill of Rights remained, it remanded funding of mental health services to individual states. That meant the country didn’t have a unified national mental health system. We still don’t have one.
Reagan also “cleaned up” the disability benefits (SSDI) program to get rid of the “freeloaders,” making it difficult for those with mental illnesses to stay on disability. It isn’t possible to conjure up mania or depression to prove to a disability claims reviewer that you’re disabled enough to warrant assistance.
Reagan’s attitude toward people with mental illnesses receiving disability services added to a growing list of stigmas. Those in the Recovery Movement used the terms mentalism and sane chauvinism to describe the public’s negative assumptions: that we’re incompetent, violent, irrational, hopeless, and, now, trying to game the system.
Despite Reagan’s evisceration of mental health funding and support, recovery and the idea that those with lived experience of mental illness had much to contribute to the mental health system started to gain traction, the Recovery Movement experienced an important but not well-publicized windfall in 1987.
The same year I was admitted to my first intensive outpatient program and my psychologist told my mother and me that I’d never recover and would likely die as a result of complications from anorexia, Courtenay Harding published the landmark Vermont longitudinal study of people with schizophrenia.
Harding was a registered nurse studying research psychology at the University of Vermont. She was tasked with following up with patients who’d been diagnosed with schizophrenia in the 1950s. A long-term psychiatric study of its kind had never been done. Schizophrenia was thought of as chronic or deteriorating at best and hopeless and incapacitating at worst. But Harding found that one-half to two-thirds had “achieved considerable improvement or recovered.”
If that was true of schizophrenia, what of other supposed chronic, hopeless disorders? Harding would later point out the grave effect of calling any mental illness deteriorating or chronic or lifelong. She writes: “These perceptions about schizophrenia have pervaded and guided clinical judgments, treatment programming, policy formulation, and decisions about priority for funding.”
We don’t recover without being given the means to do so, yet some of us, as Harding showed, somehow manage it anyway. There’s no reason it has to be this way nearly half a century later. As Harding wrote, “These perceptions have also stripped hopes of recovery from patients and their families.”
We need to start teaching young people about the recovery movement—from Pinel and Pussin to Chamberlin and beyond—showing them that along with the multiple diagnoses they may receive, recovery is possible.
Thank you for reading! You can buy my journalistic memoir Pathological: The True Story of Six Misdiagnoses (HarperCollins), a USA Today bestseller that traces how we’ve come to believe that ordinary emotions are mental disorders. If you’ve already read it, thank you! You can gift a copy to a friend, your local library, or your favorite used bookstore.
The idea that wellness is determined by whether someone can work touches on Richard Roy Grinker’s argument that the stigma against those with mental illnesses is the result of capitalism. According to Grinker, discrimination stems from biases against the disabled because some don’t have a full-time, traditional job. His book Nobody’s Normal: How Culture Created the Stigma of Mental Illness is well worth reading.




It is incomprehensible that most doctors never were interested in studying nutrition. It is the key to good health for the body and mind. They are not separate and both the body and mind need the right nutrition. As someone who has studied nutrition for a lifetime...91 years. I have experienced the result of starving the mind of the nutrients it needs...mental illness. The answer to mental illness in the past was locking up people in insane asylums. Doctors did not know anything about the causes of mental illness. The mind needs to be fed..and most people are not getting the nutrients the mind needs in our society today. The wrong food wipes out nutrients and can cause mood swings, such as, sugar. My father was a 'sugar-holic' and had a very bad temper. I didn't understand it as a child, but I learned, after I got into the study of nutrition in 1961. The first thing I did was eliminate sugar, white flour, and all additives, preservatives and chemicals in the foods my family consumed. My son who had been very hyperactive and had been put on tranquilizers... settled down and went on to graduate high school as an honor roll student. Doctors dispense drugs...when drugs destroy the human brain, lower intelligence, destroy memory, ambition and drive. Tranquilizers stunt the growing organs of children...and doctors don't seem to know this information. My son was given tranquilizers at four years of age, after the doctor created his hyperactivity with the sugar-laden diet he told me to feed the child. I followed the doctor's advice, because I was totally ignorant about nutrition. When i started reading nutrition and health books in 1961...because of this sick child...it became a lifelong search for the truth. My newsletter: Journey to Wellness. barbaracharis.substack.com
Thanks for this essay. Since you started in France, I wondered where European countries were in their attitudes toward recovery and cure.