What We Don't Talk About When We Talk About Addiction
Caffeine, sugar, and the voice in our heads
My love of sugar is deep.
At the age of seven or eight, I stole money from my mother, silver dollars she received from my grandfather, to buy candy. While the other kids played outside, I snuck away to the corner store and bought a Lik-a-Stix Fun Dip (beware of foods that drop vowels and consonants), a powdered candy you eat by licking a hard candy stick and dipping it in a magical concoction of primarily corn syrup, sugar, artificial flavors, and dyes. Never a good liar, I returned home with my lips and tongue blue from the artificial dyes and was caught in the act.
When I was about six, I received one of those toy baking ovens for Christmas, the ones where you mix the powder and water, and (somehow) a bulb cooks a mini-cake. I’d go in the closet and eat the sugary powder, coughing, trying not to be heard.
In kindergarten, I pocketed extra Flintstone vitamins for the sugar rush, trying to eat them surreptitiously on the reading rug.
When I had anorexia in my teens, my diet consisted of a perfectly measured half cup of Breyers Mint Chocolate Chip ice cream and a baked potato.
Before I started to heal from mental illness in my forties, I ate ice cream every night. A lot of it. I’ve eaten pints of absurdly expensive coconut milk ice cream, almond milk ice cream, soy milk ice cream—with pretend sugars presented as “healthy.” Agave syrup, which it turns out is worse than high fructose corn syrup. Invert sugar. Beet sugar. Brown rice syrup. Stevia. Erythritol. Monk fruit sweetener. Coconut sugar.
All forms of sugar should have been an obvious no for someone experiencing anxiety, distractibility, impulsivity, mania, depression, and panic. I’d been on and ignored enough sugar highs and glycemic lows to know that. If I’d paid attention to what happens after it hit my tastebuds, I’d feel the rush and then my heart beating in my chest.
The links between sugar and mental illness are plentiful. A 2017 study showed a link between sugar intake and depression. A 2015 study demonstrated an association between soft drink consumption and depression. In a 2019 animal study, rats that binged on sugar and then fasted were anxious. (The poor little rats. I’ve spent many nights trying to figure out how researchers knew the rats were anxious.) Sugar has been shown to suppress a hormone that people with schizophrenia may be deficient in.
The branch of medicine called Nutritional Psychiatry exists for a reason. Diet is key to mental health—everyone knows that.
Otherwise, my diet was pretty clean. One of the beneficial byproducts of the years I spent obsessing over my weight and food as someone with anorexia is that I know way too much about nutrition.
Then and today, I followed the Wahls diet, which is basically by color: green foods, orange, purple. And cruciferous. No grains. Dr. Terry Wahls cured herself of multiple sclerosis by eating three massive plates of kale every day and making sure her diet consisted of three cups of green foods, three cups of cruciferous foods, and three cups of color foods before she ate anything else each day.
I could do it because I was—and am—privileged. I lived and live in a city and have access to fresh foods. Dinner doesn’t come from a convenience store. I have time to prepare my food, not traveling and eating in airports or grabbing Chipotle on the go. I don’t have children, so I don’t have to stock chemical-laden, processed foods because fighting with my kid to eat broccoli isn’t worth it, and those foods are designed to be addictive.
So I decided to cut out sugar. Yes, honey too.
One day, I went to the freezer and threw away the two gallons of ice cream that were in there. It was something I—as an addict—had done many times, trying to quit but unable to.
Of course, once the tubs were in the garbage, it all seemed wrong. Did I really need to cut it out? Doing so seemed so extreme, so Puritan.
Other people ate sugar. Then came thoughts of x diet or y celebrity.
Yes, but other people aren’t trying to do what’s supposedly impossible: heal from mental illness.
The addiction part? I considered taking it out of the trash and eating it.
Then came caffeine.
Caffeine consumption, which I did a lot of, should also have been an obvious no.
Caffeine-induced anxiety disorder is a subtype of a diagnosis found in the Diagnostic and Statistical Manual of Mental Disorders (DSM), psychiatry’s manual. Caffeine has also been found to trigger manic episodes. And the evidence that it supposedly helps with ADHD symptoms is contradictory, leading many to believe that it makes it worse.
There’s no number of cups of coffee or cans of Red Bull that mark the amount that will trigger its negative effects, but here’s how it works when it goes awry:
The brain buzzes from the very first sip, which seems like a good thing, but that’s the complex effects of dopamine levels rising in the brain and levels of feel-good neurotransmitter serotonin falling. (Alertness doesn’t bring happiness.)
Then comes the jitteriness in the hands, the restlessness.
The heart begins to beat quickly or pound.
The sweating starts.
Maybe there’s a ringing in the ears, a sense of dislocation.
Maybe nausea, chest pain, dizziness.
Giving up caffeine should have been the first recommendation any doctor or mental health physician made, long before any benzodiazepines and other anti-anxiety meds, before mood stabilizers, before antipsychotics and all the other drugs I was on.
I’d been drinking it for years in various forms, mostly coffee and tea (black, green, etc.)—not a lot, one cup in the morning and one in the afternoon but a lot for me. No soda. No Red Bull silliness.
Before any clinician leveled a psychiatric diagnosis and told me (incorrectly) that I had a lifelong, “biological” psychiatric condition due to a “chemical imbalance,” my lifestyle should have been taken into account.
It’s pretty basic. Let’s take all the people diagnosed with anxiety disorders and major depressive disorder and mania and ADHD and have them cut out caffeine and see where we are.
So I decided to cut it out—which I’d tried to do many times and failed (hence the addiction part).
I poured my milky cup of coffee down the sink, threw away the bag of coffee grounds and then my coffee maker.
Then came the thought: Other people get to drink coffee. I’m a writer. Writers drink coffee. Or at least tea. It’s part of the job.
I thought of famous writers and their coffee.
Balzac and his fifty cups of coffee a day. (He woke at 1 AM, so there was time.) He wrote, “As soon as coffee is in your stomach, there is a general commotion. Ideas begin to move…similes arise, the paper is covered. Coffee is your ally and writing ceases to be a struggle”
And Voltaire and his thirty to forty cups.
And Gertrude Stein.
And Capote.

Never mind if I even liked these writers.
Maybe I could be like Jonathan Swift, who drank it once a week and said doing so was essential to his writing.
And I’d read Michael Pollan’s asinine book Caffeine, which basically said the world wouldn’t have been created without it.
*
Of other addictions, I didn’t smoke or drink alcohol or take illicit drugs, which put me at a distinct advantage when it came to recovery.
I quit drinking almost twenty years ago. Unlike with caffeine, it was clear to me even then that if I struggled with depression and regularly drank a depressant (alcohol), it wasn’t going to go well.
Drug use has been found to cause depression, anxiety, and psychosis. Speed (amphetamine) has been linked to a five-fold risk of psychosis. Other drugs that produce drug-induced psychosis include marijuana, psychedelic drugs like LSD, ecstasy, and MDMA. Ketamine is also known as the street drug Special K. Cocaine produces symptoms of psychiatric disorders, even in those who don’t suffer from mental illness, including agitation, paranoia, hallucinations, delusions, violence, as well as suicidal and homicidal thinking.
Knowing how hard it’s been to recover from mental illness, I’m not sure how anyone heals from co-occurring disorders (mental illness and substance use disorders).
A few years ago—post recovery—I enrolled in a one-hundred-ten-hour training in substance abuse recovery counseling.
I listened to people who quit heroin and crack and healed from mental illness, a few while living on the streets. A young woman—maybe twenty—who was a meth addict exuded a ferocity that blew my mind when she spoke of her recovery. They filled me with awe.
*
Not that healing from mental illness was easy.
Sugar was mostly mental, but when I gave up caffeine completely, the panic attacks started. My chest thrummed with an unsettling energy not just after a cup but all the time. My cheeks went numb. The room fell away. I wasn’t really there. I was dying.
Quitting caffeine was a bit like struggling with mental illness.
Knowing it’s a panic attack doesn’t decrease the panic. I’m dying. Eventually, the panic settles after what feels like a very long time.
I started negotiating with the term “quitting caffeine,” attempting to outwit the milligrams of caffeine in each substance. Coffee was out, but tea was okay. Then black tea was out, but green tea was okay. Then green tea was out, but hot cocoa is okay.
At one of my appointments with my psychiatrist Dr. R, we sat opposite each other.
I told him I was trying to quit drinking caffeine.
He bobbed his head the way he always did. “Good idea.”
My stomach sank with disappointment. I wanted him to say, Ah, don’t worry about that. A little caffeine is okay.
But he was an excellent psychiatrist—the first to tell me that diagnoses are meaningless labels meant for physicians to use, not patients to identify with, and to present recovery to me as an option.
He hadn’t volunteered that I should quit caffeine, but during that session, he agreed that no amount of caffeine is “okay.”
It still seemed unfair, like everyone else had it easy.
That was the discouraging part about mental health recovery. There was so much to give up to get well.
But there were also so much data showing people recovered and that I could too.
Though many mistakenly believe that depression is biological, chronic, and lifelong, at least a century-and-a-half of studies have shown otherwise, citing recovery rates from 49 to 76 percent.
In a meta-analysis, Samuel Guze and Eli Robins at Washington University Medical School, who actually inspired the biomedical model, found that 50 percent of people hospitalized for depression had no recurrence and only one in ten people were chronically ill.
In the 1960s and 1970s, before the Prozac-biomedical-model era, the official line from the National Institute of Mental Health (NIMH) was that depression tended to resolve itself.
One NIMH official wrote, “Depression is, on the whole, one of the psychiatric conditions with the best prognosis for eventual recovery with or without treatment. Most depressions are self-limited.”
One NIMH study saw 73 percent of patients with schizophrenia discharged after just one year and remaining in the community three years after discharge.
Another study found that 85 percent of patients discharged within five years successfully lived in the community more than six years later.
An additional study determined that of nearly half of the patients discharged in 1950, more than half never relapsed over the next four years. Overall, these studies indicated that during this pre-pharma era, only 20 percent of patients with schizophrenia needed to be continuously hospitalized.
Dr. R crossed his leg in a figure-four, bobbed his head. That was that.
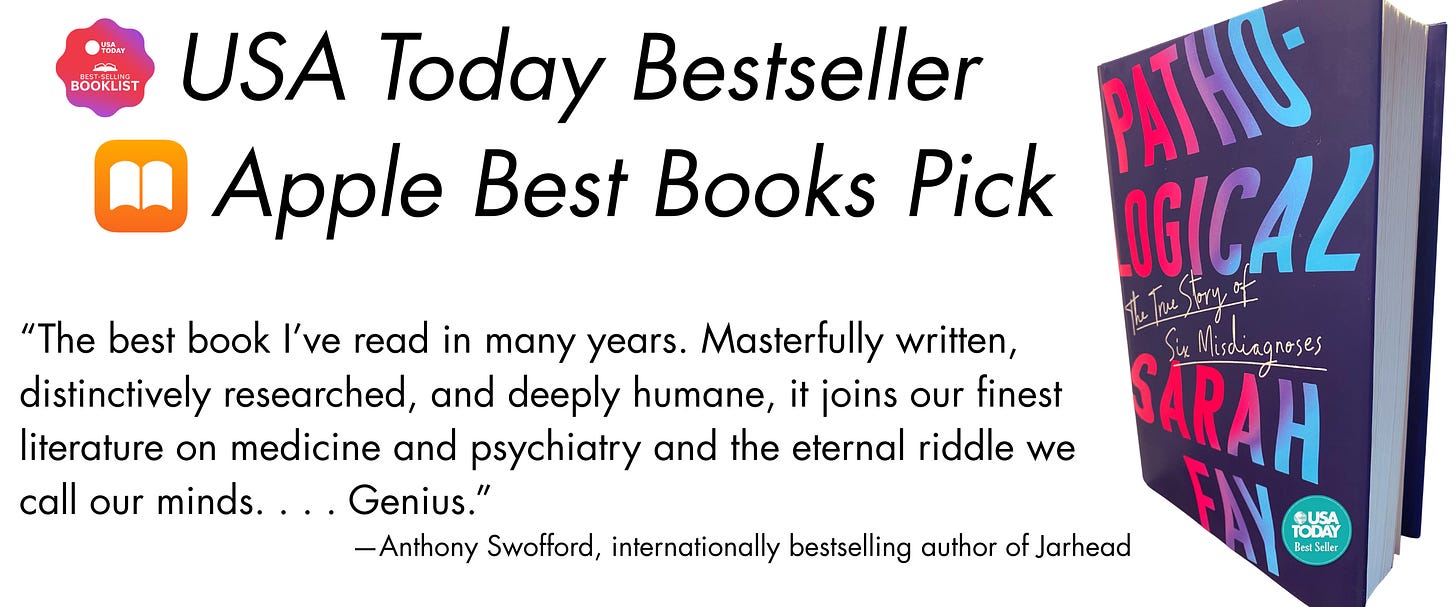
You can buy my national bestselling memoir Pathological, hailed by The New York Times as “a fiery manifesto of a memoir.”
Pathological traces how we’ve come to believe that ordinary emotions are mental disorders.
If you’ve already purchased a copy, thank you! You can gift a copy to a friend, your local library, or your favorite used bookstore.




Sugar was my first addiction too, with the same kinds of behaviors you described. It’s a beast.
A fascinating (and beautiful) piece, Sarah. Your self-discipline is truly extraordinary. (Please breathe on me, so I can catch a tiny fraction of it.)